Patient safety often depends on the quality of shift handovers. A rushed or unclear handover can lead to missed details, duplicated work, or even harmful errors.
That’s why healthcare teams are turning to the SBAR framework—a simple, structured communication tool that ensures the right information gets passed every time.
In this article, we’ll cover:
- What SBAR is and why it works
- Step-by-step: How to use SBAR in your shift handovers
- A ready-to-use SBAR template you can apply today
What Is SBAR?
SBAR stands for:
- Situation – What’s happening right now?
- Background – What’s the relevant history?
- Assessment – What’s your clinical evaluation?
- Recommendation – What needs to happen next?
The SBAR framework was first developed in the military and later adopted in healthcare to improve handover safety. It gives staff a consistent structure to follow, cutting down on confusion and ensuring every patient’s critical information is shared.
Why Use SBAR for Shift Handovers?
During shift handovers, nurses and doctors are often tired, distracted, or rushed. This is exactly when mistakes happen—important details are skipped, or instructions aren’t clear.
Using SBAR:
- Reduces errors by standardizing communication
- Saves time with a clear structure
- Improves teamwork by keeping everyone on the same page
- Boosts patient safety by ensuring continuity of care
How to Use SBAR in Your Shift Handovers
Here’s a practical step-by-step guide:
1. Situation
Start with the most urgent or current issue.
Example: “Mr. Lopez, age 65, admitted with pneumonia, oxygen saturation dropped to 88% an hour ago.”
2. Background
Share only the key medical history and relevant details.
Example: “History of COPD, on oxygen at 2L. Antibiotics started yesterday. No known drug allergies.”
3. Assessment
Give your professional judgment.
Example: “Patient is short of breath, respiratory rate is 26. Breath sounds diminished on the right side.”
4. Recommendation
State what you think should happen next or what you need from the incoming team.
Example: “Suggest chest X-ray and notify respiratory therapy for possible escalation of oxygen support.”
Read more on SBAR Proper Implementation And Best Examples
SBAR Template for Shift Handovers
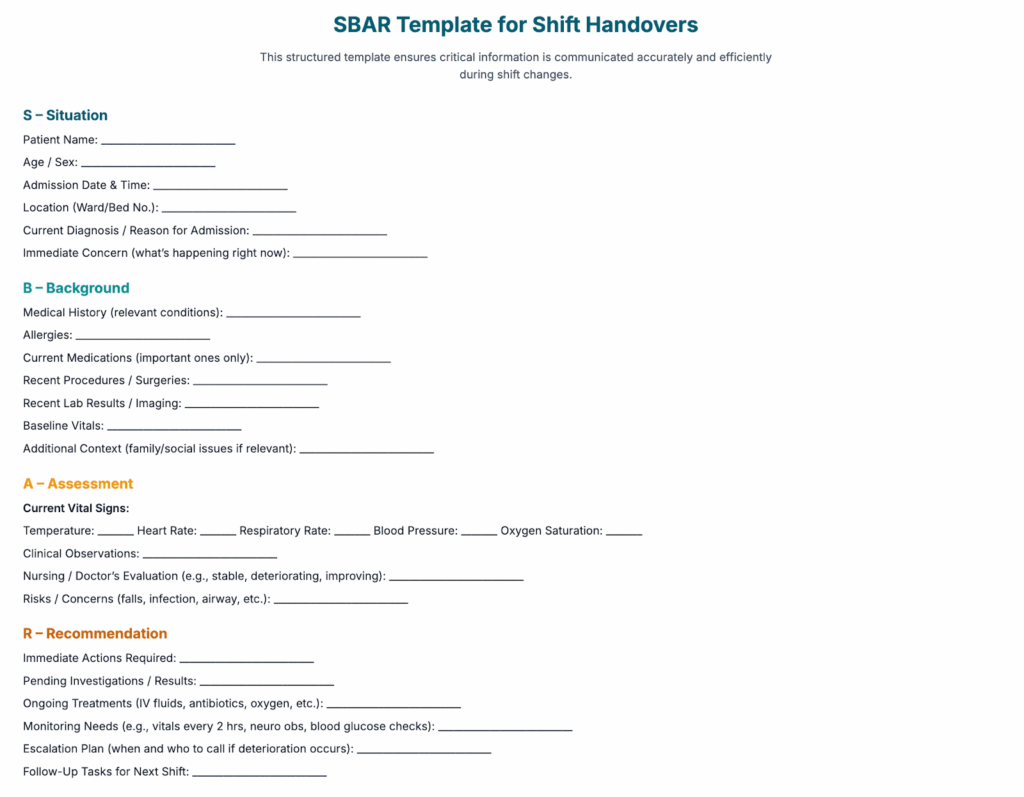
SBAR template for Shift Handovers
Here’s a simple template you can copy or print for your team:
SBAR Handover Template
S – Situation:
[Patient name, age, reason for admission, current issue]
B – Background:
[Relevant history, diagnosis, treatments, allergies]
A – Assessment:
[Current status, vital signs, clinical findings]
R – Recommendation:
[What needs to be done, follow-ups, monitoring instructions]
Pro Tip: Print this template, laminate it, and use a marker for bedside or nursing station handovers. It keeps communication structured, fast, and safe.
Final Thoughts
Handover errors are preventable. Adopting the SBAR framework gives your team a clear, reliable way to pass patient information during shift handovers. Start small—try using the template for your next shift, then build it into your standard protocol.
With practice, SBAR will feel natural, reduce mistakes, and most importantly, keep patients safe.

99win hú hú há há
Hey all, seen the jljl55phapp floating around. Is it worth checking out? Any good bonuses or games to recommend?
1666bet? Not bad, not bad at all. Their odds are competitive, and they have a good range of sports to bet on. I’ve had a few winning streaks there. Worth a look at 1666bet.
Alright, so keobet88 showed up on my radar. Checked it out and the interface is clean. Seems reliable for kèo. What do you guys think?
99boncasino https://www.99boncasino.net
premyofun https://www.repremyofun.org
[1933]LuckyPH Online Casino Philippines: Register & Login to Play Top LuckyPH Slots. Get the LuckyPH App Download for Premium Gaming and Big Wins! Join LuckyPH Online Casino Philippines! Access your LuckyPH login or LuckyPH register to play top LuckyPH slots. Get the LuckyPH app download for big wins today! visit: luckyph