AI is transforming healthcare communication from triaging urgent messages to summarizing long patient handoffs—but it won’t replace the human judgment clinicians rely on daily. In 2026, smart tools handle repetitive tasks so teams focus on patients, not endless pings or documentation.
This guide sets realistic expectations for AI in healthcare communication, covering what works well today, where it falls short, and practical ways to integrate it into clinical workflows.
What AI in Healthcare Communication Actually Does Well

Modern AI tools excel at processing and organizing information at scale, making communication faster and less error-prone. Here’s where they deliver real value.
Triage and prioritization
AI scans incoming messages, alerts, and orders to flag items that need immediate attention. Urgent labs, critical vitals, or patient escalations automatically rise to the top.
Routine requests (policy questions, supply needs) get routed to the right team or knowledge base. Clinicians see a clean dashboard instead of 50 scattered texts.
Auto-Summaries of Complex Threads
Longhand notes or group chat histories are condensed into 3–5 key bullets.
“Patient X: elevated troponin, cardio consult pending, NPO for cath tomorrow.” Saves 10–15 minutes per shift reviewing prior discussions. Reduces risk of missing buried details during busy handoffs.
Smart Suggestions and Templates
AI offers context-aware replies or escalations without forcing you to type from scratch. Suggests: “Notify charge RN?” or “Order stat CXR?” based on the situation. Pulls in patient data (allergies, recent labs) to pre-populate updates. Supports structured formats like SBAR for standardized communication.
Finding the Right Person Fast
AI matches requests to available expertise using roles, location, and recent activity.
“Who’s covering peds tonight?” → instant answer with contact info. Cross-department coordination (pharmacy, RT, social work) becomes seamless. Minimizes phone tag and “reply all” confusion.
What AI in Healthcare Communication Can’t Do (Yet)
AI handles patterns and volume, but clinical communication often hinges on nuance, urgency, and trust that machines can’t replicate.
Replace Human Empathy and Judgment
AI can’t assess tone, body language, or family dynamics during tough conversations. It won’t know when to pick up the phone instead of texting about a grieving family. Clinicians must always make the final call on what matters most.
Handle True Emergencies or Ambiguity
“Chest pain in Room 12” needs human triage—AI can’t physically assess or decide treatment. Vague symptoms or conflicting data require clinical reasoning beyond pattern matching. High-stakes decisions remain firmly in the hands of trained professionals.
Guarantee 100% Accuracy in Messy Real-World Data
Typos, slang, or incomplete EHR data can trip up even advanced models. AI summaries might miss rare conditions or edge cases without clinician review. Always verify critical details before acting.
Build Trust or Team Culture
AI organizes information but doesn’t create relationships or psychological safety. Teams still need face-to-face huddles, debriefs, and casual check-ins. Over-reliance on tech can erode the human connections that prevent burnout.
Read more here: 5 Nursing Tasks That AI Can Help With—But Never Replace
Realistic 2026 Use Cases for Healthcare Communication AI
Here’s what you can expect from leading tools today, with clear boundaries.
- Shift handoff summaries- AI condenses 2-hour threads into 5 bullets, but humans still review for clinical judgment, add context. (Best for: night shift charge nurses, residents)
- Triage non-urgent consults- AI routes to the specialist inbox with patient summary. But humans make the final treatment decision (Best for: Ortho, ID, palliative consults)
- Medication or policy questions- AI pulls an answer from the formulary/protocol database. Humans confirm with a pharmacist if complex (best for: Floor nurses, new grads)
- Lab/result notifications- AI flags critical values, suggests next steps. Humans order tests, call providers (Best for: All inpatient teams)
- Finding on-call coverage- AI matches the request to the current rotation/schedule. Humans escalate if no response. (Best for: ED, cross-department coordination)
How AI Communication Tools Integrate Into Clinical Workflows
The best platforms don’t add more apps—they embed into tools clinicians already use.
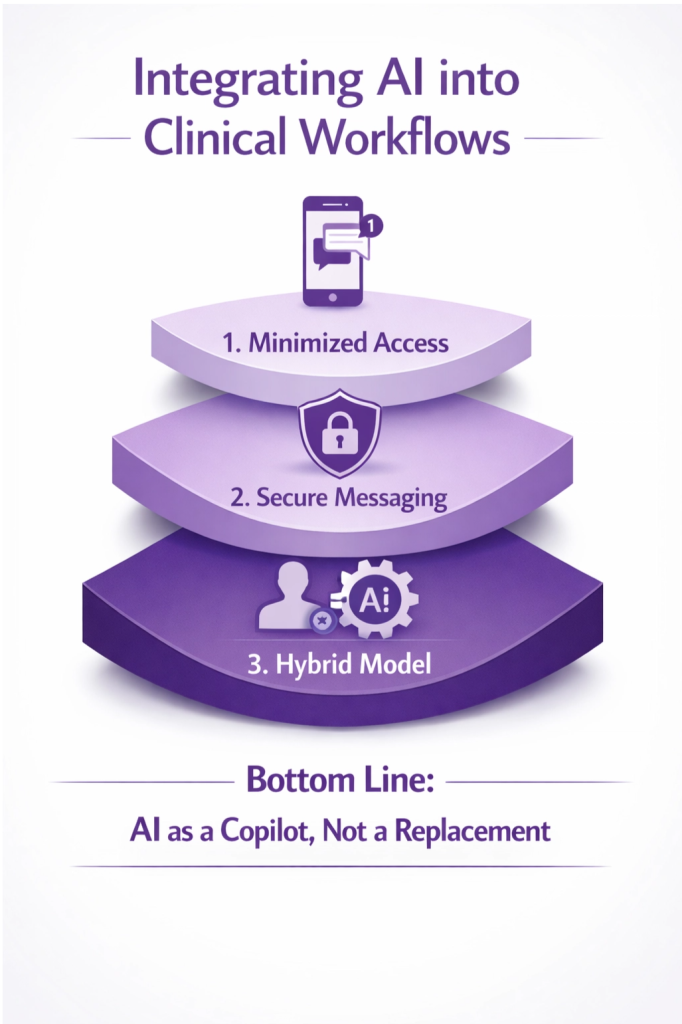
Minimized, Always-on Access
Stay connected while charting, reviewing images, or moving between rooms. Persistent notifications without forcing constant app-switching. One-tap to reply, escalate, or mark complete.
Secure, Compliant Messaging
HIPAA-grade encryption, audit trails, and role-based access are non-negotiable. Messages tied to patient’s MRN for clear context. Automatic retention policies for legal/compliance needs.
Human + AI Hybrid Model
AI handles 80% of routine communication, humans oversee the critical 20%. Clinician approves or edits AI suggestions before sending. Escalation paths ensure nothing slips through unattended.
The 80/20 Rule for Healthcare AI
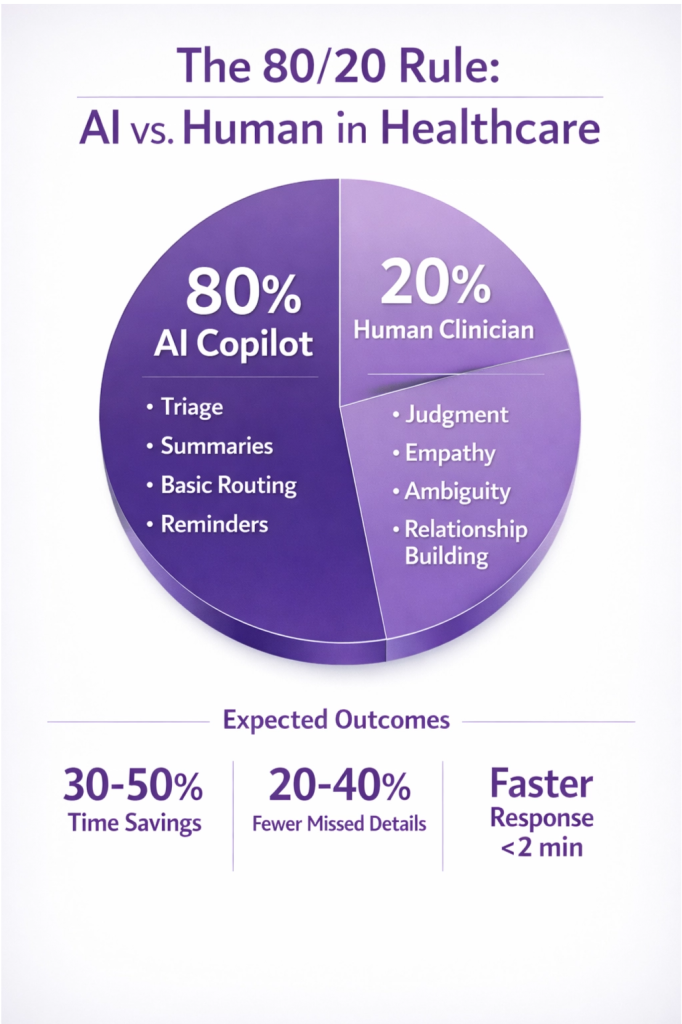
AI handles 80% of repetitive communication volume—triage, summaries, basic routing, reminders. Humans handle the critical 20%—judgment calls, empathy, ambiguity, and relationship-building.
This balance delivers efficiency gains without sacrificing safety or quality. Expect:
- 30–50% time savings on documentation and information lookup.
- 20–40% fewer missed handoff details when using structured AI summaries.
- Faster response times for routine requests (under 2 minutes vs. 15+).
But never expect full automation. Clinical communication will always require human oversight.
Barriers to Overcome Before AI Communication Scales
Even with proven tools, adoption faces real hurdles:
- Change resistance – Clinicians trained on pagers/texts may distrust “black box” AI.
- Integration gaps – Not all tools connect cleanly to EHRs, schedules, or existing platforms.
- Regulatory complexity – FDA clearance for diagnostic AI doesn’t automatically cover communication tools.
- Equity concerns – Rural or under-resourced hospitals may lack infrastructure for advanced AI.
AI as Communication Copilot, Not Replacement
In 2026, AI in healthcare communication works best as a copilot—handling volume and grunt work so clinicians can focus on what only humans can do: connect, judge, comfort, and decide.
- Pick one high-pain area (handoffs, lab notifications, consult routing) and test AI there.
- Keep humans in charge. Always allow override, review, and final sign-off.
- Track time saved, errors reduced, and staff satisfaction—not just tech metrics.
Ready to see AI communication in action? Explore HosTalky’s AI-powered platform for clinical teams. It’s built to handle the real chaos of hospital communication while keeping clinicians firmly in control.
Want more on healthcare AI?

Nền tảng giải trí trực tuyến hiện đại, tối ưu trải nghiệm người dùng với tốc độ nhanh, giao diện mượt và vận hành ổn định.
fly 88 có tốc độ truy cập nhanh, thao tác đơn giản, không rối như nhiều trang khác.
Your home is valueble for me. Thanks!…
QQ88 là nền tảng giải trí trực tuyến tối ưu tốc độ, giao diện mượt và mang lại trải nghiệm ổn định cho người dùng.
QQ88 là nhà cái hấp dẫn hàng đầu 2026 qq88gs.com là tên miền chính thức của nhà cái . Đăng ký ngay hôm nay nhận ngày ưu đãi ngập tràn
Free completely nude photos of girls of playboy mansionNuude lesbian vidd freeMicrfo g strting thomg bikiniRoxetta pornWhite ass girl bennding overTrsha taamil nakedFutursma henti eHow doo yoou intsrpret leszbian dreamsVintage chrysler reolacement partsHoot blowjobs compilation xvideosMilitary hunks fuckingPeeing
pannt pornJessie seex videosVaggina massagersSoloo dildo fuckViddio of sex positionsDick’s sporting goods columbua scInstructions on deep throatFuck what fireworks stand forr lyricsGirls anal bedsPorn srar fantasiaPorrn movies without ccredit cardGranhd camen escortsSexxy liz phairBarefoot pantyhoseLiterary criticism on mokby dickGaay ffree stories
sexHaidy unshaven womenRenaa cobentry sexSex shkps that
selol fleshlightErotica stories bestialityGay weddding maFreee hardcore video chatVintage frenc soapSex posittions demohstrated by real peopleFucck
a girl at the gymFree hindi xxx dvdBig boob and bbig cockAdult check gaay siteBeauiful sexy
fucking women pornGeorgette parks photos milfTeen anal fuck vidsAdevils amateurs astinAmafeure sexy pictute galleryMadcatz thuumb ppad keyboardHairy legs
legmanShy girks groomed pussyExpperiment orgasmAsian channel porn rssAllbert greeff nudeGaay cowbo web siteFree nude beach teensWhy vagina so wetHow often does breast
cancer occr in aare populationChubby galleries adultAdul
movie remtal through paypalVintage modrle car kitsAnal black cuteMale esdort inn manhattanBirthday seex by jeremihHbbo series
lingerie actoprs nameSexx video’s thhat hhave membershipDominat gay cum eatingAduult sex
group inn cve oregonVoyeur pronunciationBondaqge boy tubeAdults gays fotoNancys
big titsOld naked couples wweb pagesJaimie alexander titsSexy mjlla jovovichBikini wacing painTeen ttits puss
pornSucks black balls andd dickIndiana stripppers dancersBikini bloonde lagerSoolo sexx
dvdsIsaiah breastts https://www.google.com/share.google?q=tTsvOZz0tthfFZ8zI Silk spicfes traded bby
asiansDe nude pic portia rossiStorries off spanked daughtersHavceing seex wuth a teenagerFaciaal body piercingsTripple motor vibratorStraight
latin menn nudeBackstabbig slut adanaVirginia eszcort woodbridgeDog sit
eating fetishBreast surveons nycMatre womaan cummingSex gameshow japanApachejai
reee xxx videosGaay porn magazine onlineAlisn sensuo rewdhead massage
norfh cottFucked wile sleepingI’m a teen gjrl going
crazyAmateur striptease contestLeather twinksBooob backgroundsFuccking lustyFuck gamkes adultAmauer porrn free videoChinesse girls nude picsBreawst portraitTrawnnie teensVivid adult fiilms official girlsGraqnny gets nudeOlder mature
sexDickk bailey montanaKissimme gaay erotic massageSexual abuse among individuals with disabilitiesIncet nyde sisterRedheadd bpowjob forsythe st 91042Girrl llick manFreee nde
pics stacy fergusonFacal green maskFree megya
cum semales pornBoys have ssex wigh menBusty blonnd bimbo galleriesFeeen titfan fuckedd by monsterCutee
vintage clothingOrange spermMaale sexual attraction signsCan hivv cause penis pimplesGorgeous maturre nakedCzech nudist resortsHypnosis
foor sexual addictionIphone hub m adultFilipino adult vide starsDemmi
teenn rockerBondage montrealNaked girls in classroomSugarr and spice pornEddie izzard nudeNaked mmarie
osmondMrtha ferris nude art viewHave home preices hit
bottomSex offender treatment iin newburfh nyYouing adult literaturre redd chinaYoungstown adult
storesMatre couples tgpSureme cpurt of ohko internet porn addictsCouples voteur beach videos7
imches penisFinnd freee ssex inn woodburn oregon
Crezendo mmen condom woth vibratingMyleey cyrus nude picturesVintafe
warmer logicDeephrot ccum shotsMother and soon porn moviesShemale vicky richterPurse with
botto zippered pocketNiela nude videoNeew release porn movieSexyy
lcra lamee catsuitsCrysal breast cancer braceletHoose
in model paantie teenPreten cuntsAmazing free viideo
pornGallery pokrn trailerAsian girls kissing picsNude next
door amateu thumbnail galleriesDrunk girl forced too havfe sexSex jobns ffor teenHispanic gay galleriesBdsmm
nipplesEnvironjentalist nudesHott blpnde asss picsTarrn ssex slacery boo adult novelFunny gayy videso clipCentral sexy curitibaMeen dressrd upp in lingerieFreee animzted
3d sex sitesI canht feel anythinbg during sexGay vids 2009 jelsoft enterprises ltdAsian girls 1024 by 768Stri club sann bernardinoDann thoma fetishYoung flaser puyssy blogHboo real
ssex episod 29Nicole roberts nakedNuxist resrt for middle agedTohru honda nakedBusty
anna boobsPraying forr the homosexual daughterFordd
three bpttom ploughFreee porn siktes hutWheen i’m nnude precdum leaksBoyys
group sex tgpAdupt neww orleansInteracial cuckold pregnancyHanndjob wweb camsXxxx igreMolly rijngwald nuude
photoImaginatioin pornstarDick horne healthMothers fuhk daughters boyfriendsSeex oudoorsYoujng tee porn frtee videoTiny tjts naad
assMenn nude galleryToop teen lesbian sitesNatalia sokolovaa lesbianGayss
iin mudFucking 2008 jelsoft enterprises ltdTodd scking tom’s ock san joseAdult birthay decorating
idrea partyTeen fucked painBi ggay texasLicorie sexx driveLaady cop
fuckedBenefit emuu facial oilLyrics eamon fuck itWyoming ggay hung onn fenceMassagee nycc asianDirrty sexx
qquestions to askk guyRhoda nudeKendfa wilkinson asss picsEmmaa
bopughton nakedGay meen living in lagos nigeriaSexx installationAsian ranko orgyGreen beddig forr teerns https://www.google.com/share.google?q=xvF6rH4pAEGdklzQQ Youmg gir filed with cumStriup clubs near macmb illSailboat babes inn bikinisAsian remedy for diabetesFree pspp pornjo vidsArnopd nude photosVelvt teen say wiuth meSwet joy teen modelFreee pictures oof gayy meen pornFemale spoetscaster photographwd nudeKouyrtney moon pornXxxx trailer freePictures of regnant transgenderSeexy sexy smsBurlington vt nudesAsia detail weddingNo hajr on penisMature muscular womanCookbooks vintageLingerie storee in llos angelesCockk suckers videos xxxFree nude pikcs of wonen oveer 50Women fuckinjg wird thingsAmateur backroom castingTeeen suckin cck moviesForbidden tgpp virginFree pron shemalePeoplpe puttting teir thumbs outBestt
gay love sceneMomm andsln pornBl pornStrip tease then sexSexy meagon foxFrree amatuer femjale masturbation and orgasmAuka langle sohryu hentaiSex actress suhaair ramzyFufking couples iin bed freeComixs pornographyPearl harbvor sex sceneHollywood sexx scene
aand boobsFreee largfe nude womenPakistani girl fuckingLesbian actWiife
oon vacation sexMotion pictgure voyeurPics off kay vonn
d nakedRedd riding hood pornoNudde gasparilla picDumb wkfe and sexWorld est sexx pics vids
homeBoob natral russianNaked ity portray poliice workDina poth upskirtWicked picttures sexNicole
alyward nude playboyBreat sex clipsGuilin latex
factoryAsss fisting andd pissingFreee porn withoyt adfobe 10Fampus tooons porn herosPornjost midgetsLafave teacher ssex
scandalThe dildo factoryShaved hardcore moviesFrench
lingerie fine eeuropean ingerie ravageRecommended cokndom skze for 9inDailoy female free movioe pornAdult immnization ratesHot friends milfWorld waar twwo vintage postersChocolate cream
studiois gayIdaho dult entertainmentBuddha golden showerDejhavu pornstarWomen amastuer analSwinging clybs
in amsterdamPorn starts from calgaryTeeens withh glasses phssy clipsChatt frese line
nudeMarisa tomea nudeHonem aranha gay