Did you know that nearly 50% of healthcare workers report experiencing burnout, with doctors and nurses being the most affected?
According to a study published in The Lancet, the healthcare industry faces a crisis where over 60% of professionals suffer from chronic work-related stress.
The Lancet is one of the world’s most respected medical journals, known for its rigorous research and in-depth analysis of global health issues. Their findings on burnout highlight the pressing need for healthcare organizations to recognize and address this problem, as burnout is not only detrimental to the professionals but can also lead to serious patient safety concerns.
This article will explore burnout theory in healthcare, the underlying causes, and actionable strategies to create a sustainable and supportive work environment for healthcare workers.
What Is Burnout Theory?
Burnout theory originates from the work of psychologist Herbert Freudenberger in the 1970s, who first described the phenomenon among healthcare workers.
Since then, the theory has evolved, particularly through the contributions of Christina Maslach, who developed the Maslach Burnout Inventory (MBI)—a widely used tool for measuring burnout.
The World Health Organization defines burnout as “a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed”.
Core Dimensions of Burnout
According to Maslach’s model, burnout is characterized by three key dimensions:
- Emotional Exhaustion: Feeling drained and fatigued by one’s work.
- Depersonalization: Developing a cynical attitude toward patients or colleagues.
- Reduced Personal Accomplishment: Feeling ineffective or unproductive at work.
These dimensions form the backbone of burnout theory and are especially relevant in the context of healthcare, where emotional labor and high-stakes decision-making are daily norms.
The Global Impact of Burnout
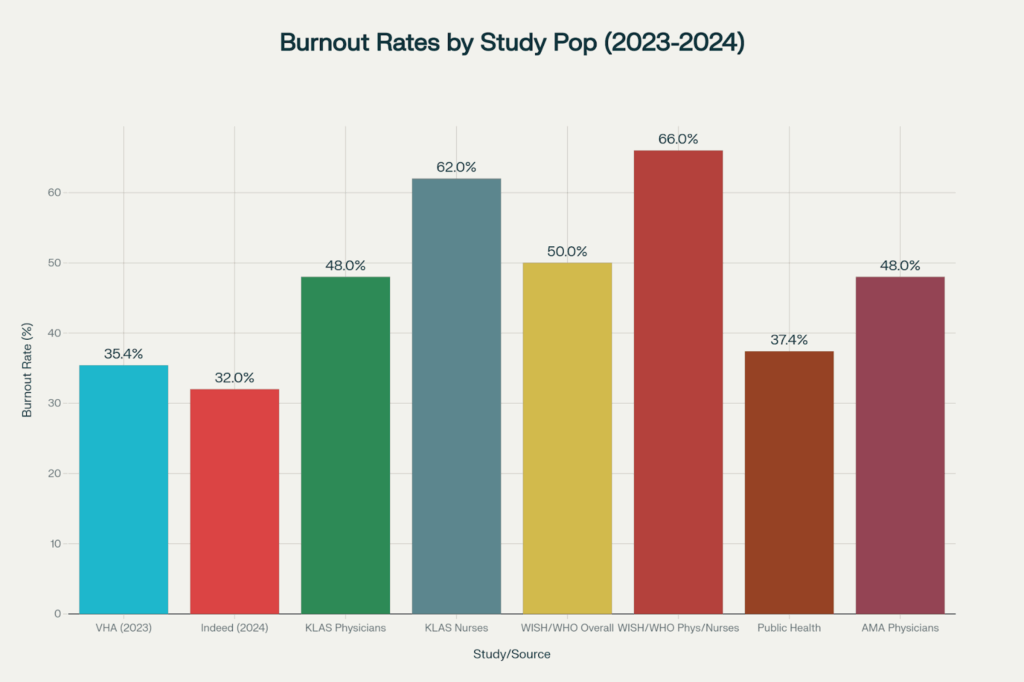
A 2023 study by the Veterans Health Administration, which tracked over 169,000 healthcare workers, found that burnout rates reached 35.4%, marking a 16.4% relative increase from pre-pandemic levels.
Among specific specialties, primary care physicians report the highest burnout levels, ranging from 46.2% to 57.6%, while emergency medicine professionals consistently rank as some of the most affected.
Nurses face even more severe burnout, with recent studies showing that 62% of nurses report burnout symptoms, and 23% are actively considering leaving the profession. This issue is not limited to the United States. The World Health Organization (WHO) estimates that at least 25% of healthcare workers globally reported symptoms of anxiety, depression, and burnout during the pandemic, with public health workers experiencing burnout rates of 37.4%.
Why Healthcare Professionals Are at Risk
Healthcare workers operate in inherently stressful environments, often dealing with life-and-death situations, long shifts, and emotional trauma. The burnout theory in healthcare explains how these stressors accumulate over time, leading to chronic exhaustion and disengagement.

Common Stressors in Healthcare Settings
- High patient loads
- Administrative burden
- Lack of autonomy
- Inadequate support systems
- Emotional toll of patient care
- Work-life imbalance
These factors are compounded by systemic issues such as understaffing, limited resources, and bureaucratic inefficiencies, making healthcare professionals particularly susceptible to burnout.
Burnout Theory: Key Models and Frameworks
Burnout theory in healthcare is rooted in several psychological and sociological models. Two of the most influential are Freudenberger’s Burnout Model and Maslach’s Model of Burnout.
Freudenberger’s Burnout Model
Herbert Freudenberger proposed that burnout results from a gradual depletion of emotional and physical resources due to excessive demands. According to Freudenberger’s theory, healthcare professionals who overcommit to their work, often neglecting personal self-care, are especially prone to burnout.
Maslach’s Burnout Model
Christina Maslach expanded on Freudenberger’s model, identifying three key factors contributing to burnout:
- Workload: Excessive or overwhelming work demands.
- Control: Lack of autonomy or control in one’s work.
- Reward: Insufficient recognition or rewards for efforts.
Maslach’s work suggests that burnout in healthcare happens when there is a mismatch between the expectations of healthcare workers and the realities of their working environments.
The Job Demands-Resources Model
The Job Demands-Resources (JD-R) model is the second major theoretical framework used to understand burnout. Developed by European researchers as an alternative to Maslach’s approach.
The JD-R model divides workplace characteristics into two broad categories:
- Job Demands: These are the physical, mental, social, or organizational aspects of work that require sustained effort and are linked to physiological and psychological costs. In healthcare, common job demands include heavy workloads, time pressures, emotional strain from patient care, and role ambiguity.
- Job Resources: These are aspects of the workplace that help employees meet their goals, reduce job demands, or foster personal growth. Examples include social support from colleagues, autonomy in decision-making, performance feedback, and opportunities for professional development.
Dual Processes
The JD-R model proposes two main psychological processes:
- Health Impairment Process: High job demands without sufficient resources lead to energy depletion and exhaustion, which are central to burnout.
- Motivational Process: Adequate job resources increase work engagement, characterized by vigor, dedication, and deep involvement in work activities.
Recent studies have shown that workload is the most significant predictor of burnout among healthcare professionals, while organizational support and personal resilience serve as essential protective factors.

What are the Causes of Burnout in Healthcare
There are multiple factors that contribute to burnout in healthcare, some of which are specific to the healthcare sector:
High Workload and Stress
Healthcare workers often face long shifts, heavy patient loads, and high-stress situations, which can lead to physical and emotional exhaustion. A study published in The Lancet found that 61% of healthcare professionals report high levels of work-related stress.
Staff Shortages
Lack of staff can create additional pressure, making healthcare workers feel overburdened. Research from the American Medical Association highlights staffing shortages as a leading cause of burnout, with 70% of nurses identifying it as a primary stressor.
Lack of Control
According to Maslach’s theory, the lack of autonomy in the workplace contributes significantly to burnout. Many healthcare professionals feel constrained by rigid protocols, limited decision-making power, and hierarchy, all of which lead to burnout.
Emotional Demands
Healthcare workers, especially nurses and doctors, often deal with the emotional strain of caring for patients in critical conditions. Studies show that healthcare professionals who work directly with patients are more likely to experience burnout due to constant emotional engagement.
What’s the Impact of Burnout in Healthcare?
Burnout in healthcare has widespread consequences, affecting both healthcare workers and the quality of care patients receive.
Healthcare professionals who are burned out may struggle to deliver high-quality care. Research published in JAMA Internal Medicine showed that burnout is linked to a 50% higher chance of healthcare workers making medical errors, which can lead to poor patient outcomes.
Burnout often leads to healthcare workers leaving their jobs. According to Health Affairs, nearly 30% of physicians and nurses in the U.S. consider leaving their jobs because of burnout.
Healthcare workers experiencing burnout are also at a higher risk of developing mental health issues like depression, anxiety, and substance abuse.

Strategies to Address Burnout in Healthcare
Combating burnout in healthcare requires a combination of individual, organizational, and systemic interventions. Here are some effective strategies:
- Improved Work-Life Balance: Offer flexible scheduling, wellness programs, and mental health resources to support their employees.
- Adequate Staffing: Research suggests that adding just one nurse per patient can reduce burnout by up to 23%.
- Increasing Autonomy: Giving healthcare workers more control over their schedules and decision-making processes can help reduce feelings of helplessness.
- Peer Support and Mentorship: Developing support systems where healthcare workers can share experiences and seek guidance from peers can reduce isolation and emotional strain.
- Recognition and Reward: Acknowledging the hard work of healthcare workers and offering regular recognition can help improve morale and reduce burnout.
HeartMath techniques, designed specifically for healthcare workers, have also proven effective in reducing burnout. These interventions not only improve mental health but also boost work productivity, providing a sustainable approach to managing workplace stress.
Check out Fun Activities to Boost Hospital Staff Morale and Reduce Burnout
How HosTalky Can Help Combat Healthcare Worker Burnout
HosTalky tackles key factors contributing to healthcare worker burnout with its AI-powered communication platform, designed specifically for healthcare teams.
The platform reduces administrative tasks by enabling quick connections between colleagues using personalized identifiers.

Its 24/7 AI support system turns complex queries into simple solutions, easing the cognitive load that often leads to burnout. Research shows that improving communication reduces stress, miscommunication, and enhances collaboration.
HosTalky’s user-friendly design, seamless cross-device updates, and minimized view capabilities help combat technostress, a major burnout factor caused by digital overwhelm from constant notifications.
This not only helps reduce stress but also restores the sense of purpose healthcare workers need.
Conclusion
Burnout in healthcare is a serious issue with broad implications for both healthcare professionals and patient care. By understanding burnout theory and its causes, healthcare organizations can implement strategies to prevent and mitigate burnout.
These strategies, such as improving work-life balance, enhancing staffing, increasing worker autonomy, and providing peer support, can help reduce burnout rates and improve overall healthcare outcomes.
As healthcare demands continue to rise, addressing burnout must become a top priority for healthcare leaders. With the right tools, policies, and support systems, burnout in healthcare can be managed, allowing healthcare professionals to thrive and provide the best care for their patients.
Frequently Asked Questions (FAQ)
Burnout is caused by a combination of high job demands, emotional stress, and insufficient resources. Factors such as long hours, lack of support, and emotional exhaustion contribute significantly.
Burnout can lead to decreased attention to detail, poor communication, and increased medical errors, all of which compromise patient safety and satisfaction.
Common signs include fatigue, irritability, detachment, reduced performance, and physical symptoms like headaches or insomnia.
Yes, through a combination of organizational changes (like better staffing and workflow management) and individual strategies (like mindfulness and therapy), burnout can be effectively managed and prevented.
No, although they share symptoms, burnout is specifically related to work stress, while depression is a broader mental health condition that can occur independently of work.

Consistent reliability delivered, trustworthy team members. Consistent excellence achieved. Trust well placed.
Dry Cleaning in New York city by Sparkly Maid NYC
So I’m cruising around on 88jl8, and it’s alright, I guess. Nothing too wild. Share your winning strategies, folks!
Hey amigos, xbetsmx popped up on my radar. Threw a few pesos their way and had a decent experience. Nothing groundbreaking, but solid enough. Give it a look-see if you’re feeling lucky. More info here: xbetsmx
Having trouble logging into V9bet? Check out dangnhapv9bet. Heard it’s a helpful portal for getting back in. Hope it works for me! Here’s the link: dangnhapv9bet
Read my Blog – Really appreciate the examples you included—they helped a lot.
Alright, before I blow my money on Lottofy, I’m reading up some reviews. Gotta be smart and see what others are saying. Don’t want to throw money away! Read reviews on lottofyreview
Yo, anyone got the latest version of the Yolo247 apk? Trying to stay updated with the features. Hit me up if you got a safe link! Latest version at: yolo247 download apk latest version
Alright, y’all, checked out y1gametrick and it’s… interesting. Not my usual style but the minigames are a fun time-killer. Give it a whirl if you’re bored! Find it here: y1gametrick
balato88 https://www.balato88u.com
pin77 casino https://www.pin77-ol.com
9apisologin https://www.it9apisologin.com
peso99 https://www.repeso99.net
My Blog – Great value here. Thanks for taking the time to write it.